The medical benefits of mild electrical stimulation of the cranium may seem like marketing hype, but decades of clinical research studies have verified that it does alleviate symptoms in a wide range of conditions. This method delivers very-low-frequency current to electrodes placed on the head, and that tiny current spreads across the brain to influence neurons and affect brain-network connectivity. Today, psychiatrists and neurologists commonly employ this technique as part of the therapy for people with anxiety, depression, post-traumatic stress disorder, epilepsy, Parkinson’s disease, and a host of other conditions. Researchers are also reporting that stimulation can improve mental performance.
Part of the reason for the excitement around cranial electrical stimulation is its use of such low-level current—typically just 1–2 mA—that it carries virtually no side effects [1], [2]. That makes it an attractive and essentially no-risk option to try for therapy either in the clinic or at home, or for research into brain networks and associated behavior.
Taking It Home
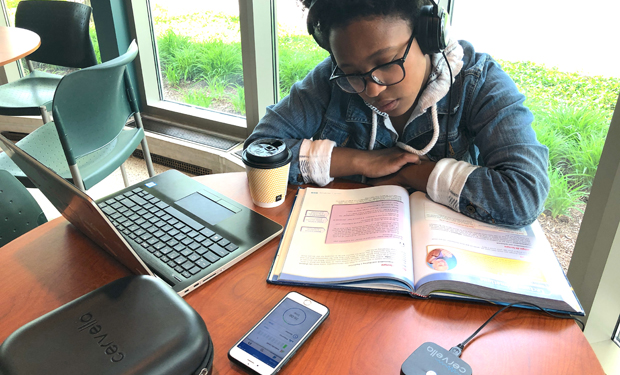
A growing number of companies are fabricating new devices to deliver the stimulation either by direct current [transcranial direct current stimulation (tDCS)] or alternating current (tACS). One of the latest is the Cervella device, which received the U.S. Department of Food and Drug Administration’s market clearance for treatment of depression, anxiety and insomnia in March 2019 [3]. Offered by Innovative Neurological Devices LLC of Carmel, IN, Cervella uses as little as 50 μA of ac delivered via over-the-ear headphones, described company CEO Bart Waclawik (Figure 1). “The headset ear cushions use proprietary conductive cloth, and that’s how we make the electrical contact with the mastoid area,” he said. The device also uses conductive water-based gel applied at the point of contact to improve the electrical flow through the skin and to the cranium and brain, he added.

Waclawik, already an experienced medical- device developer, became interested in cranial electrical stimulation when one of his young family members needed help dealing with diagnosed general anxiety disorder but was experiencing severe adverse events from drug-based therapy. Waclawik started looking for solutions, and came across tACS with both its well-documented efficacy and lack of contraindications and adverse effects.
Waclawik gave his relative one of the commercially available tACS devices to try. “The condition improved, and the acute anxiety attacks were severely diminished,” he recounted. Nonetheless, his relative soon quit using the device because the clips hurt his ears, and he felt embarrassed using it in public. Waclawik and company engineers began work on an alternative, and after polling other young users and hearing similar complaints, they designed a device that was comfortable and inconspicuous. “We decided to integrate the electrodes into the earpads of high-quality, noise-canceling, Bluetooth headphones that patients can use anywhere and nobody would know,” he said (Figures 2 and 3).
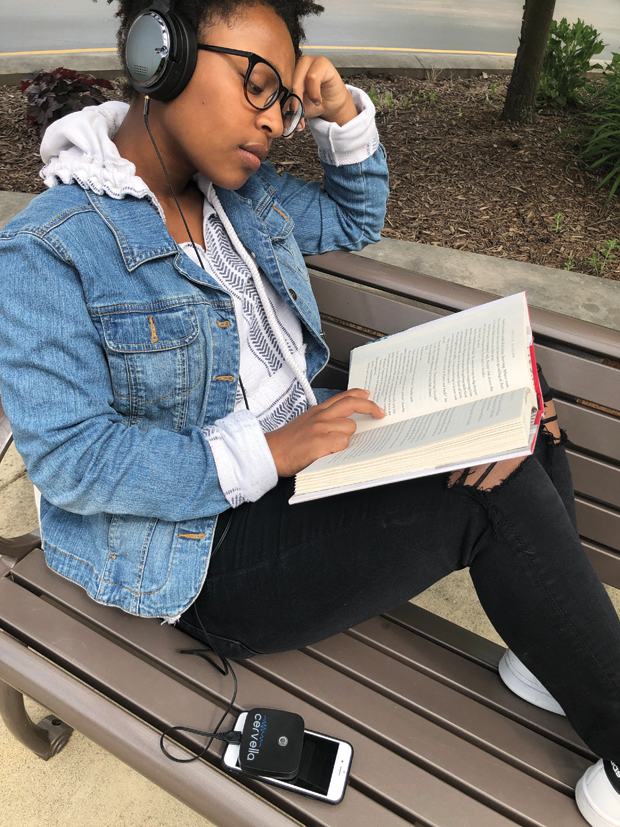

Besides the headset design, Cervella also offers other innovations. One is patient control of certain parameters, notably the intensity of the stimulation, which is adjustable in 50-μA increments to account for variability in skin resistance between individuals. With the intensity adjustment, users hone in on the point where they feel a faint tingling sensation, which indicates the device is doing its job, Waclawik said. Another innovation is an app that automatically records patient-use data. Providers can then access that data to understand patient use and progress, and to manage treatment.
While enthusiastic about tACS, Waclawik is careful not to oversell it. “The efficacy is 50%–60% with these devices, but we don’t want to come across as saying this is a panacea and this will treat everybody. This is another tool in the physician’s toolbox, and the good news is that because it doesn’t have contraindications with drugs or other therapies, it can be used in conjunction with them, so we are leaving the application of this device to the discretion of the health care professional,” he said. Shipment of Cervella in the U.S. is planned for July 2019.
Medical supervision is indeed an important component of home-based care and so is ease of use, according to tDCS researcher Marom Bikson, professor of biomedical engineering at City University of New York (CUNY). He is also cofounder of Soterix Medical of New York City, which is developing tDCS for home, clinical, and research applications. On the medical-supervision side, Soterix is working on an automated home system that a clinician (or researcher if it’s part of a research project) can monitor and direct via telemedicine (Figure 4). “There’s a lot of technology that goes into that, including reliable communication between the technology and the site that’s providing the telemedicine, as well as automated software that can collect information from the patient on a daily basis, and can also deliver the prescription that the doctor sets,” Bikson said. “Although the software doesn’t decide what the treatment will be, it can withhold treatment until the patient is ready to receive it based on the doctor’s prescription schedule.”

To make the home device simple to use, Soterix has already designed and developed “Snap Pads,” which are electrode-equipped sponges that come pre-moistened to facilitate the passage current through the skin and to the brain. A few of the many engineering challenges included selecting sponge material that would hold sufficient moisture for the current transfer, but would neither drip nor dry out during a stimulation session, and designing packaging that was easy to open and pads that were simple to snap onto the device’s headgear, even by tDCS users with dexterity issues. “These were not trivial things,” Bikson said. “Even with apparently simple- to-use devices, you need technology that is optimized for the job.”
Going High-Def
Besides the home-based tDCS system, Soterix also developed something quite different for use in research labs and clinics: targeted tDCS that delivers current to precise, small areas of the brain, as compared to the 5×5-cm areas covered by each of the two pads or sponges seen in typical home-based systems, Bikson explained. The idea with targeted tDCS is to personalize treatment for individual patients and/or to reduce distinct symptoms.
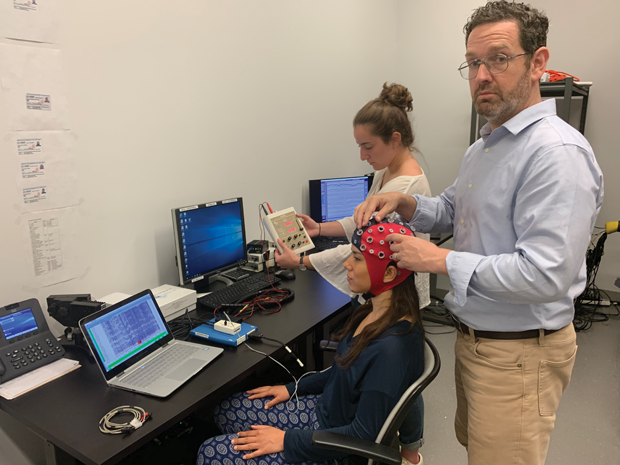
Soterix actually engineered the first noninvasive, targeted, and low-intensity neuromodulation technology, dubbed high-definition tDCS (HD-tDCS), back in 2009. “HD-tDCS and its variants, which include HD-tACS, use an array of smaller electrodes to stimulate specific parts of the brain,” Bikson said. He portrayed Soterix’s HD-tDCS as looking like “a swim cap with little knobs on it” (Figure 5). Each knob is a gel-based, high-definition (HD) electrode that is connected by a wire to a stimulation box. Soterix also developed neurotargeting software to pinpoint the proper location of the electrodes on the scalp, and to turn on or off each electrode individually to control the spatial distribution of the applied current.
Bikson’s CUNY research group is pursuing the notion of personalized medicine and individualized stimulation with two goals. One is to analyze patient tDCS data and responses as a way to identify which individuals are most likely to benefit from brain stimulation. “This has very important implications for clinical trials and efficacy,” he asserted. The other is determining how to personalize the stimulation for individuals so each patient receives optimal benefits. “Currently in TDCS trials, everybody gets the same stimulation,” he remarked. “The question is, can we move beyond that, and can we—for each person on each day—be tweaking their stimulation, seeing how they respond, and then using that to inform the strategy accordingly. Those are areas I’m very interested in not just from an engineering perspective, but also because I believe that could have a huge impact on efficacy. ”

One of the groups already using HD-tACS to personalize stimulation is that of researcher Robert Reinhart, Ph.D., director of the Visual Cognitive Neuroscience Laboratory and assistant professor in the Department of Psychological and Brain Sciences at Boston University (right). He and his research group have shown that targeted HD-tACS can impart cognitive improvements to older adults. In this work, which was published in Nature Neuroscience in April 2019 [4], they focused on working memory, or the higher cognitive ability that supports everyday functions, such as language, decision-making, facial recognition, and general navigation. They were especially interested in the brain’s temporal cortex and prefrontal cortex, which are involved in storing and processing working-memory content.
For the experiment, subjects donned an HD-tACS skull cap outfitted with a half-dozen ring electrodes, each 12 mm in diameter and arranged at key locations on the cap (Figure 7). “We used alternating current because it allows the possibility of rhythmically tagging certain brain wave frequencies that are thought to have functional significance, and as a result manipulate a specific brain network and behavior,” Reinhart explained. This also allowed them to match each subject’s distinctive natural brain rhythms.
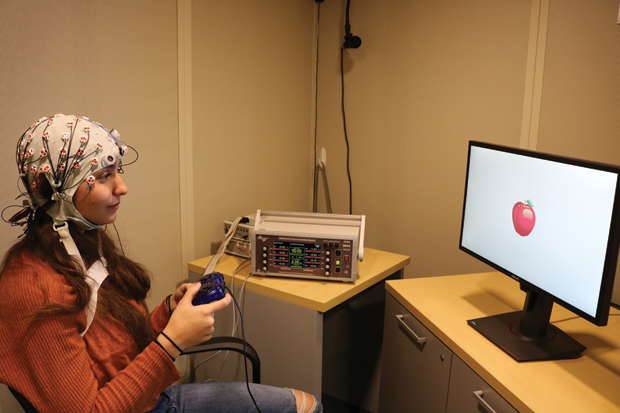
They then observed 84 healthy individuals— half of them in the 20–29 age bracket, and half in the 60–76 range—while performing a working-memory task. This involved showing each subject two similar pictures three seconds apart, and having them report if the two pictures were the same or different. The older group noticeably under-performed compared to the younger group (80% vs. 90%), as was expected. The researchers followed up by applying targeted HD-tACS—25 minutes of very low intensity stimulation (1.6 mA)—to the older individuals. “After brain stimulation and relative to a variety of shams (the tingling sensation without actual stimulation), we saw the older people boost up to 90%, so it was just like the 20- year-olds,” Reinhart said.
“We were also interested in brain-communications motifs, which are the ways the brain communicates with itself through rhythmic patterns of brain activity,” he said, pointing out that the prefrontal and temporal areas show different neuronal firing actions that are linked (known as theta-gamma phase amplitude cross-frequency coupling). “This theta-gamma coupling occurs during working memory maintenance,” he said. To study this aspect, Reinhart’s group also monitored electroencephalograms of the subjects as they performed the working-memory task, and found better synchronization of rhythmic activity between the prefrontal and temporal regions of the brain when the patient was receiving personalized stimulation.
They found no improvements in performance or synchronization when they used nontargeted HD-tACS. He summarized, “This work showed that space, frequency, and personalization were all important in being able to generate the changes we saw in working memory behavior and brain activity.”
Additionally, older subjects continued to do better on the working-memory task for the entire period of the experiment, which ran for 50 minutes after they received HD-tACS. “I have a grant submitted now to test the duration effects, and we’re going to go out to 200 minutes and even to the next day, because we want to know when they wear off,” Reinhart said.
More to Come
Waclawik, Bikson, and Reinhart all believe brain electrical stimulation will become an even bigger part of medical care in the future. “One reason is that people are sick of being over-medicated and they’re looking for some alternative approaches,” Waclawik said, adding that the ability to combine stimulation with other therapies makes it a very attractive option.
Reinhart agreed that stimulation has great potential when used in combination with other therapies. “There are a lot of findings accumulating now that should give people hope and optimism about potential ‘electroceuticals,’ or ways to target electrical circuits in the brain and repair them, especially as an add-on or adjunct approach to traditional pharmacology, psychotherapy, or whatever other technique it could be paired with to exploit the plasticity of the brain and make the effect of those techniques more potent and long-lasting.” The potential is also there for stimulation to be used as a replacement therapy, he added. “It seems like it’s opening up a new avenue of treatment options, especially for those people for whom traditional treatments are just not working.”
Reinhart and his group are also investigating the concurrent stimulation of multiple brain regions to study other questions of connectivity. “That’s important because there are a variety of conditions, such as autism, Alzheimer’s, and schizophrenia, that show decreased connectivity; and other conditions, such as epilepsy, anxiety, and Parkinson’s that show too much connectivity,” he remarked. “The implications of this tool are that you may be able to up- or down-regulate functional connectivity in these disorders, so it has the potential to be really helpful as a clinical application one day.”
The possible clinical implications of stimulation are tremendous, Bikson remarked, and that is especially true of tDCS, which is the most extensively studied of the electrical stimulation technologies. “Because tDCS has been grounded in so much animal and human research, I believe it has a lot of potential to effect human health,” he said. “If only 1% of the indications that tDCS is being tested for get broadly used clinically, it would be a transformative technology. As far as new treatments for neurological and psychiatric indications go, there’s a lot to be excited about.”
References
- M. Bikson et al., “Safety of transcranial direct current stimulation: Evidence based update 2016,” Brain Stimul., vol. 9, no. 5, pp. 641–661, Sep.–Oct. 2016.
- H. Matsumoto and Y. Ugawa. “Adverse events of tDCS and tACS: A review,” Clin. Neurophysiol. Pract., vol. 2, pp. 19–25, Dec. 2016.
- U.S. Food and Drug Administration, “510(k) premarket notification,” Mar. 2019. Accessed: May 28, 2019. [Online].
- R. M. G. Reinhart and J. A. Nguyen, “Working memory revived in older adults by synchronizing rhythmic brain circuits,” Nature Neurosci., vol. 22, no. 5, pp. 820–827, Apr. 2019.