Researchers are using organoids derived from stem cells to study neurological diseases, learn about human development, and develop potential treatments for disorders
Measuring just a millimeter or two in diameter, brain organoids are a far cry from a fully functioning human brain. But these miniature tissues, typically derived from stem cells, are increasingly able to mimic the structure and function of our most complex organ, unlocking exciting possibilities for neuroscience, artificial intelligence, and beyond.
“In many ways, the brain is still a black box,” said Alysson Muotri, Ph.D., a professor in the Departments of Pediatrics and Cellular and Molecular Medicine at the University of California, San Diego. “There are fundamental questions—such as how the brain works, how cortical networks form, what inputs and outputs occur during development—that we have no idea about. Organoids can help us answer those questions.”
Powerful tool for disease modeling
First described in 2008 by Japanese stem cell biologist Yoshiki Sasai, Ph.D., brain organoids were initially used to explore open-ended questions about how neurons respond to stimulation and whether standalone neural systems can be coaxed to perform specific actions [1]. In recent years, advancements in hardware, software, neurocomputational understanding, and synthetic biology have led to a series of breakthroughs in the field that set the stage for much more sophisticated investigations. “We’re suddenly seeing barriers that previously were impediments starting to be chipped away,” said Brett Kagan, Ph.D., chief scientific officer at Cortical Labs, a biological computing startup in Melbourne, Australia.
With better technology and a more nuanced understanding of the brain’s physiology, researchers are building organoids that increasingly mimic the structure and function of the human brain. Brain organoids have now demonstrated complex neural oscillations characteristic of an adult human brain. Researchers have also developed organoids that combine several types of brain cells, mimic various regions of the brain, and can mature through numerous stages of human development.
Brain organoids are quickly becoming a powerful tool for modeling neurological disorders and diseases [2]. The tissues can mimic the molecular changes, circuitry problems, and other hallmarks of a disorder, then provide a test-ground for potential treatments, such as drugs or gene therapy.
Muotri and his colleagues have studied Pitt-Hopkins syndrome (PTHS), a rare genetic disorder caused by a mutation in the TCF4 gene that leads to significant impairment, including developmental and intellectual disabilities and seizures. The researchers collected cells from children with PTHS and their parents, who did not have PTHS, then created organoids for both groups. In the PTHS organoids, they observed problems with neural progenitor cells that prevented healthy cortical development (Figure 1).

Figure 1. Alysson Muotri, Ph.D., professor in the Departments of Pediatrics and Cellular and Molecular Medicine at the University of California, San Diego, uses organoids to understand neurological diseases, brain development, and more. (Photo courtesy of Muotri Lab/UC San Diego.)
Then, the researchers tested a gene therapy approach, using a virus to deliver the corrected TCF4 gene to the underdeveloped organoids. The problems reversed—and the PTHS organoids were soon indistinguishable from their controls [3]. The technology has now been licensed and is heading into clinical trials later this year. “So far, I’m very optimistic and very positive, because all the diseases we have studied are reversible at the organoid level, which is a great example of the brain’s plasticity,” Muotri said.
Bennett Novitch, Ph.D., a professor of neurobiology and director of the Integrated Center for Neural Repair at the University of California, Los Angeles, and his colleagues have created organoids that mimic the neural activity patterns seen in Rett syndrome [4], a developmental disorder caused by an imbalance of neural excitation and inhibition, as well as epilepsy (Figure 2). Among other approaches, Novitch and his team are using assembloids, which fuse multiple organoids together to study how they differ and interact, to better understand how neurological diseases affect distinct parts of the brain.
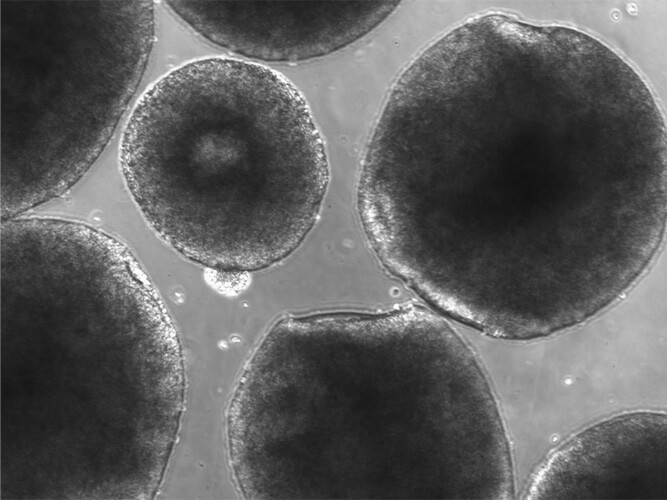
Figure 2. Organoids developed by the Muotri Lab are sent to the International Space Station to study the impact of microgravity on astronauts’ brains. (Image courtesy of Muotri Lab/UC San Diego.)
In research currently under review, they developed assembloids with a genetic mutation that causes both a severe form of epilepsy and learning and memory deficits. They then observed how the mutation impacted two different parts of the organoid: one part that resembled the brain’s cortex and another part that resembled the hippocampus. The cortical region showed massive and abnormal neural oscillations—activity that looks like seizures. The hippocampal region had relatively normal oscillations but showed changes in the activity of different circuits—ones that are distinctly hippocampal and known to be associated with learning and memory. For the first time in an organoid model, their research shows that genetic disorders manifest differently in different regions of the brain.
“We also now have an understanding of what goes wrong in hippocampal neural circuits in this particular disorder, which gives us some new ideas about how we might be able to intervene,” Novitch said.
Repairing and exploring the brain
Organoids have proven utility to model diseases and learn how to treat them—but can they also be used as treatments themselves? At the University of Pennsylvania’s Perelman School of Medicine, Han-Chiao Isaac Chen, M.D., an assistant professor of neurosurgery, is exploring whether organoids can be used as a substrate to repair the brain after a traumatic injury. Because cells in the cortex are highly organized, he and his colleagues believe that organoids may lead to more successful transplantations than standalone cells, which have been used in past trials. “The brain is a very ordered and structured system,” he said. “To truly repair it after an injury, we need to do more than just add more cells—we need those cells to have some sort of architecture.”
Chen and his team transplanted organoids into the rodent visual cortex to test how the tissues integrate with a host brain. They observed both structural and functional integration: When light was flashed in the animal’s retina, cells in the organoid were activated. The researchers also found that certain neurons in the organoid exhibited feature selectivity (they responded to specific types of light, but not others), mimicking how the human visual system works [5].
Before transplanting organoids into humans, though, Chen said clinicians need tissues that more closely resemble the human brain, along with a better understanding of how the integration process works and how to control it. “What we’ve shown so far is that integration is possible,” he said. “What we don’t know are the rules that govern that process.”
Beyond modeling and treating diseases, organoids can also provide other key insights about the brain (Figure 3). Muotri and his colleagues are working with NASA to send organoids to the International Space Station to study the impact of microgravity on astronauts’ brains. Their efforts build on earlier research in animal models, as well as cognitive tests in humans, that have found problems with learning and memory following a trip to outer space. Studying organoids may allow the researchers to understand the mechanism behind those deficits by searching for changes in cell migration, the number of synapses formed, the complexity of neuronal organization, and neural activity.
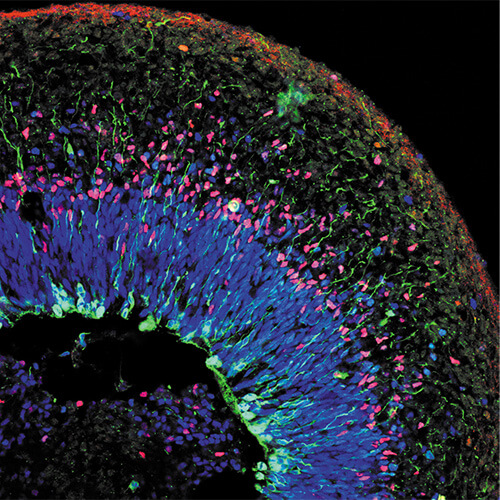
Figure 3. At the University of California, Los Angeles, Bennett Novitch, Ph.D., and his colleagues use organoids to map how neurological disorders such as epilepsy differentially impact different parts of the brain. (Image courtesy of Bennett Novitch/UCLA.)
Muotri’s team is also using organoids to compare the neurodevelopment of modern humans to other species, including chimpanzees and Neanderthals. “Since we don’t have cells from Neanderthals, we’re using genome editing to resurrect extinct mutations that are very unique,” he said. “By placing those mutations in the brain organoids, we can have insights into how their brains worked.” Their data shows that Neanderthals’ brains matured faster than human brains in the earlier stages of development, which may have conferred a survival advantage [6].
Getting closer to the brain
Research on brain organoids so far is promising, but it could be even more impactful if certain technical and scientific limitations are overcome. For one, organoid research is not always reproducible—sometimes cells grow and thrive, while others on the same protocol starve and die—and researchers don’t know why. These issues could be caused by external variability we don’t yet understand, so more robust protocols are needed.
Organoids that are cheaper, more similar to the human brain, and can grow larger and stay alive for longer could also fuel more sophisticated research efforts. At Cortical Labs, Kagan and his team built a biological computer chip that combines neurons with silicon (Figure 4) and demonstrated that the system can learn how to play a video game [7]. The baseline technology could be used to fuel diverse types of organoid research, from drug testing and disease modeling to insights about how intelligent systems form. “Can these be a tool to investigate ways to build better machine learning, or even be used themselves as a sort of intelligent system?” Kagan said. The startup is also working directly with bioethicists and philosophers to preemptively consider ethical conundrums inherent to organoid research, such as what language to use to describe the technology and whether it could one day become conscious.
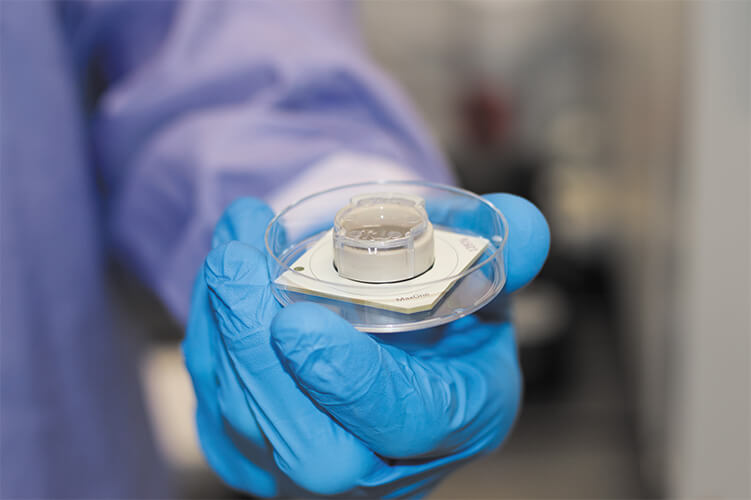
Figure 4. Cortical Labs, a startup based in Melbourne, Australia, has developed a biological computer chip that combines neurons with silicon. (Image courtesy of Cortical Labs.)
Muotri and others are also working to add vascular systems to organoids, which would provide nutrients that could fuel the growth of more cells and complexity. Currently, organoids cannot grow larger than about 5 million cells, or about half a centimeter in diameter.
In the meantime, scientists are continuing to use existing technologies to expand our understanding of diseases affecting hundreds of millions of people around the world. Organoids in outer space undergo accelerated aging, which is providing Muotri and his team with a model for late-onset diseases such as Alzheimer’s. Closer to home, Novitch is part of a new multicenter project, funded by the National Institute of Mental Health, to use organoids to study schizophrenia, depression, and a number of other neuropsychiatric conditions. They plan to systematically mutate hundreds of genes linked with those disorders and observe the effects on brain development in organoids, which may ultimately lead to a platform for drug development and screening.
“As a field, we’re continuing to work to reproduce every possible element of the healthy human brain—as well as the diseased or disordered brain—and then harness that information to ameliorate these disorders,” he said.
References
- J. Mariani and F. M. Vaccarino, “Breakthrough moments: Yoshiki Sasai’s discoveries in the third dimension,” Cell Stem Cell, vol. 24, no. 6, pp. 837–838, Jun. 2019, doi: 10.1016/j.stem.2019.05.007.
- O. L. Eichmüller and J. A. Knoblich, “Human cerebral organoids—A new tool for clinical neurology research,” Nature Rev. Neurol., vol. 18, no. 11, pp. 661–680, Oct. 2022, doi: 10.1038/s41582-022-00723-9.
- F. Papes et al., “Transcription factor 4 loss-of-function is associated with deficits in progenitor proliferation and cortical neuron content,” Nature Commun., vol. 13, no. 1, May 2022, Art. no. 2387, doi: 10.1038/s41467-022-29942-w.
- R. A. Samarasinghe et al., “Identification of neural oscillations and epileptiform changes in human brain organoids,” Nature Neurosci., vol. 24, pp. 1488–1500, Sep. 2021, doi: 10.1038/s41593-021-00906-5.
- D. Jgamadze et al., “Structural and functional integration of human forebrain organoids with the injured adult rat visual system,” Cell Stem Cell, vol. 30, no. 2, pp. 137–152, Feb. 2023, doi: 10.1016/j.stem.2023.01.004.
- C. A. Trujillo et al., “Reintroduction of the archaic variant of NOVA1 in cortical organoids alters neurodevelopment,” Science, vol. 371, no. 6530, Feb. 2021, Art. no. eaax2537, doi: 10.1126/science.aax2537.
- B. J. Kagan et al., “In vitro neurons learn and exhibit sentience when embodied in a simulated game-world,” Neuron, vol. 110, no. 23, pp. 3952–3969, Dec. 2022, doi: 10.1016/j.neuron.2022.09.001.