Simply put, an intelligent hospital is one that works better and smarter. It’s better because it’s resourceful, creative, and perceptive about what patients and doctors need, and it’s smarter because it’s astute and inventive when it comes to weaving together diverse technologies to enhance patient care. Driven not only by new regulatory requirements but by financial constraints and reductions in staff that require us to do more with less, institutions must now reevaluate their operational processes at all levels. And, while technology is important in an intelligent hospital, it’s not the only focus. Facility design is also critical, including infrastructure and room design conducive to optimizing the management of patients, supplies, and devices.
The concept of the Intelligent Hospital™ (the term “Intelligent Hospital” is a trademarked term; however, it is simply referred to without the symbol in the remainder of this article) began in 2009 as an initiative from the Radio-Frequency Identification (RFID) in Health Care Consortium. The intent was to promote education and simulate today’s technologies while, at the same time, demonstrating the integrations that enable the creation of a seamless patient care environment. The overarching goal is to create a hospital that will bring today’s smart technologies to bear in all areas, including the emergency room, operating rooms (ORs), intensive or acute care areas (ICUs), treatment areas such as radiology and radiation oncology, as well as specialty areas, including central supply, pharmacy, and biomedical engineering.
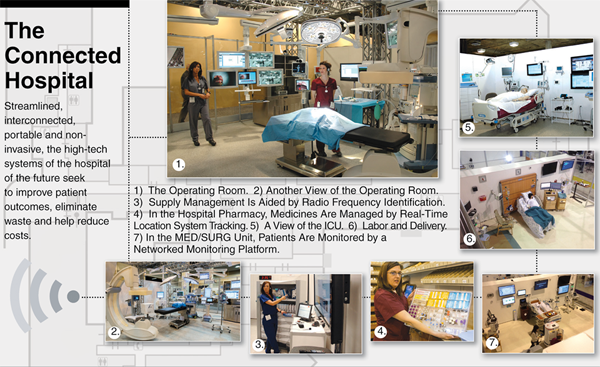
Room by room, department by department, this article describes what an intelligent hospital looks like.
Throughout the Hospital
The fundamental component of the intelligent hospital’s operation is a seamless blend of multicarrier cellular and Wi-Fi services. This critical component is key for many of the new technologies and applications and provides the medium for the rapid and broad availability of information throughout the hospital. Such a high-performance wireless network enables enhanced information exchange and real-time communications for the many various users. Once it is archived, aggregated, and available on the network infrastructure, the information can be filtered, analyzed, and presented throughout the hospital on a combination of displays, on smart devices, and in reports available within the hospital’s information systems. All clinicians can then use a variety of mobile handheld and wearable devices to readily review, communicate, and deliver critical information, including device alarms and clinical or lab data. These devices are commonly integrated into the hospital phone system, allowing incoming and outgoing calls directly from the point of care, thereby increasing the availability of staff at bedsides.
To accurately share data from multiple systems and devices, the intelligent hospital relies on a Wi-Fi-based time synchronization and Environment of Care compliance system using Network Time Protocol (NTP). This guarantees that all clocks, NTP-enabled systems, and medical devices are synchronized throughout the entire hospital to provide an accurate consolidation of data.
In addition to the high-performance networks, the intelligent hospital infrastructure also incorporates real-time continuous environmental surveillance, monitoring key environmental parameters such as temperature, humidity, airborne particulates, differential room pressure, air quality, light, and sound. The data from these sensors provide analytic information used for infection control, facilities management, and patient safety. Real-time alerts are generated any time a potentially hazardous or undesirable condition is detected, allowing for immediate response and remediation. This monitoring enables critical devices, such as freezers, to be continuously monitored, ensuring regulatory compliance as well as the integrity of critical specimen or laboratory samples.
The Operating Room
Today’s ORs often provide a hybrid surgical environment, integrating imaging modalities with surgical tables, advanced optics, light-emitting diode surgical lighting systems, and a variety of information platforms (see “The Connected Hospital”). Images from integrated high-definition camera systems, the hospital picture archiving and communication system, as well as patient demographics and status from the electronic medical record (EMR), are routed to a variety of displays within the OR and are available anywhere in the institution for consultation.
[accordion title=”The Connected Hospital”]
[/accordion]
Additionally, a hybrid OR is designed to support multiple surgical modalities and incorporates minimally invasive surgical platforms, including endoscopic devices, video cameras, lights, insufflators, and scopes, all mounted on booms to support advanced laparoscopy equipment and procedures. The OR incorporates RFID-based supply management for high value and general supplies, tracking the supplies used during the procedure and validating that all supplies are current with no specific U.S. Food and Drug Administration recalls, which significantly enhances patient safety. RFID-coupled instruments and sponges enable confirmation of item counts, ensuring that no undesired surgical devices are retained within the surgical field. All RFID-coupled supplies and medication are automatically documented in the patient record, providing an accurate representation and cost accounting of the surgical procedures.
The Patient’s Room
Patients lie in an instrumented smart bed providing a secure dynamic environment capable of monitoring patient weight as well as side rail and wheel status. The bed is integrated with a nurse call platform, providing patient-to-staff communication. Caregivers and staff wear RFID-coupled identification badges that use infrared, ultrasound, or low-frequency radio-frequency technology to provide room-level, bed-level, or better image resolution throughout the hospital and patient rooms. RFID coupled with the nurse call functionality enables workflow metrics to be monitored, optimizing the response to patient care issues. Critical patient calls and alerts, such as “bed exit” or “rails down,” can be immediately directed to the appropriate and available caregiver through the staff-worn or handheld wireless devices, including voice-over-Internet Protocol phones and pendants. In emergency case alerts in which care providers are unavailable, the system can transmit an alert to the secondary caregiver who accepts the alert and attends to the situation.
In rooms with patients who need specialized care, such as the ICU, patients are typically monitored by a networked monitoring platform. This provides real visualization and continuous monitoring of the patient’s heart rate and ECG rhythms, blood pressure, and oxygen saturation, which could be then be available in centralized monitoring and reviewing areas such as the wall of knowledge, war room, EMR archiving, and alarm management systems. These specialized locations combine information from many sources, providing a continuous and historical overview of the patient’s physiological status and condition. This monitoring platform integrates with the hospitals network infrastructure, wired and wireless, enabling continuous monitoring at all locations in the hospital. The ICU commonly uses many life support, treatment, and monitoring devices or solutions to manage the patient. All are time synchronized and integrated through a connectivity solution that allows patient-centric data to be aggregated and archived in the EMR.
In rooms designed for noncritical patient care, such as the step down, med/surg, or labor and delivery rooms, patients traditionally only have vital signs spot-checked at four-hour intervals. This often leaves these patients at risk for complications of respiratory failure, hemorrhage, and falls associated with trauma and weakness. Telemetry and new technologies such as bed sensor pads provide an alternative, enabling the system to automate the vital sign collection. Alerts can be sent to a variety of mobile devices, resulting in quicker intervention to prevent potential complications.
From Emergency Room to Intensive Care and Beyond – Connectivity and Interoperability
As patients are more closely monitored, they are typically connected to an increasing number and variety of devices including ventilators, infusion pumps, and cardiac output devices. It is vital that the data from these discrete devices and systems be time synchronized and aggregated to provide a comprehensive view and interpretation of the patient status and condition. For medical devices to share data and integrate with other applications, such as alarm management systems or the EMR, a confirmed patient-centric identification and association of devices from patient to care provider is required. This identification and association can be barcode or RFID based.
Once associated, these aggregated medical device data are archived and available anywhere inside or out of the hospital to provide analytics vital to the patient’s treatment. For critical life support devices such as ventilators, patients can be centrally or remotely monitored as alerts are delivered directly to the care provider at the point of care. This application also enables the hospital to dynamically monitor all ventilated patients independent of their location, providing a virtual ventilator community and ensuring a standard level of safety across the facility.
Real-Time Location Systems Solution
Increasingly important to the optimizing of hospital operations is the integration of RTLSs that provide unique identification, location, tracking, and association of the institution’s critical assets, including patients, safety, devices, and inventory. If we consider the processes associated with patient care and management, there is a consistent need for establishing a unique identification and association of patients, staff, devices, supplies, samples, and pharmaceuticals. Integrating RTLS-based solutions provides a basis for establishing a standardized methodology that can be applied in a variety of areas, including ventilator management, nurse call, alarm management, staff communications, sample collection, archiving, and medical administration (see Table 1).
[accordion title=”Table 1. Real-Time Location System Applications and Use Cases”]
Implementing a real-time location system (RTLS) enhances safety, optimizes workflow, manages supplies, and validates processes, providing a new level of business intelligence in the hospital’s operations. Outlined below is a subset of the many RTLS applications, which would typically be deployed in a health care environment.
Passive RFID Applications
- Supply management and tracking
- Surgical tray tracking
- Surgical sponge and instrument tracking and verification
- Pharmaceutical—medication administration
- Laboratory sample collection and archiving
- Small devices/inventory
- Patient-centric identification and association
- Verification of process
- Cleaning or decontamination processes
Active RFID Applications
- Inventory management
- Locating and tracking critical devices
- PM compliance
- Distribution of costs
- Asset utilization
- Shrinkage–security
- Workflow and management
- Staff tracking
- Identification and association
- Hand hygiene compliance
- Metrics on dynamic time sequence of events
- Dashboards
- Event generation—staff duress
- Integration with biomedical data base
- Optimization of processes
- Temperature and humidity measurement
[/accordion]
In addition, RTLSs enable the direct monitoring, confirmation, and validation of many discrete processes associated with patient care, such as hand hygiene compliance, providing an increased level of patient safety through enhanced compliance and reduction in errors.
Specialty rooms, such as the pharmacy, rely on these technologies to ensure that physicians’ orders are exactly formulated and tagged, loaded in the medication carts or pneumatic tube systems, and routed and tracked, ensuring a timely and validated delivery of medication to the correct unit and patients. These checks and balances and process validation enhance patient safety and directly reduce the potential for medication delivery-related errors.
[accordion title=”Ongoing Hospital Innovation in the Developed World”]
by Shannon Fischer
From London to Seoul, Austria to Australia, hospitals throughout the developed world have been hard at work streamlining information technology and automating their day-to-day operations to cut down on staff workloads, medical errors, and all the unnecessary complications of the modern hospital system. Even though much of the work remains in its earliest stages, positive effects are already rolling in as seen in the examples here.
Italy: Up until a few years ago, the Rizzoli Orthopaedics Institute in Bologna (see figure below) used an archaic system of paper records, despite being the country’s premier center for orthopedic surgery. The institute began a complete overhaul of its system in 2008, introducing integrated electronic medical records accessible throughout the hospital. The last part of that has been the surgical system, which formally wrapped up just last year and now boasts a fully digital monitoring system for all surgeries, incorporating World Health Organization safe surgery checklists, and real-time tracking of every step of the actual operation—from the initial planning to the arrival of the patient in the room (via sensors embedded in their wristbands), anesthesia, incision, and even materials used—all the while gathering data for analysis down the line. “That’s the future,” says hospital Medical Manager Maurizia Rolli. “We are starting to use this big amount of data and trying to go deeply in the knowledge of what is going on in our operating rooms.” And while it’s still early in the process, the institute has already uncovered sources of inefficiencies in operating room layouts and scheduling that they are beginning to address.

Spain: Hospital La Fe in Valencia, Spain, is one of the busiest medical centers in the country, juggling more than 1,000 beds, 6,000 professionals, and an average of 700 emergencies every day. To help handle the onslaught, the hospital needed to find a way to modernize data entry and care for the caregivers at the front lines—the nurses. The solution they created is a small fleet of 72 Mobile Nursing Workstations, piloted in 2009 and then rolled out to the entire hospital system starting in 2011 (Figure S2). Each station is an ergonomic, Wi-Fi-equipped cart armed with medication storage, touchscreen computer interfaces, radio-frequency identification scanners to identify the patient, and devices able to monitor such vitals as blood oxygenation and pressure, temperature, and heart rate, and then send all of the resulting data automatically into patient electronic health records. The expected savings from this data transfer as well as from the improvements in patient care that the carts have created—medication safety, shorter diagnosis delays, and more reliable monitoring—sum to €1 million per year.

Australia: Systems Architect Matt Darling got a close-up look at the inefficiencies of hospital systems as he sat by his daughter’s bedside in a Sydney hospital six years ago. Data were entered multiple times on various paper forms before they went into a computer, harried nurses sometimes pre-emptively filled out charts before treatments were administered—which meant that missed doses often went unnoticed—and the existing software systems were clunky, complicated, and gave no assurance that the actual data were entered correctly (after a dose was given) or not.
In the years following his daughter’s death, Darling devised a comprehensive solution to the problems he witnessed: a streamlined information system called SmartWard that includes bedside data entry stations and geospacially enabling tokens on staff, patients, and medications. When a health care professional nears a patient’s bed, the system automatically pulls up key details such as patient identity and proposed treatment. If they’re carrying the wrong medication, an alert pops up; if they’re interrupted before they can give a correct treatment, another alert sends a heads-up to other nursing staff and ensures that the task isn’t marked as complete until the medicine is actually administered. And no less remarkably, the entire thing can be tweaked as needed for far less effort than a traditional system. Between the first two testing phases, 57 changes were requested, all completed for just US$20,000—a fraction of the US$10 to 20 million Darling estimates a standard electronic medical record system would have required. “What we’ve implemented is not just an application, but a systems ecosystem that enables us to make changes to the logic without affecting the architecture,” Darling says.
Initial trials with nursing staff at two of Melbourne’s Eastern Health hospitals found that the system more than halved the amount of time nurses spent on documentation, tripled the time they could spend interacting with patients, and increased the amount of data entry at patient bedsides—as opposed to back at the nurses’ stations—by 60%. The system is now under consideration for deployment in more than two dozen hospitals in Australia. And since SmartWard is actually designed to function hospital-wide, Darling expects its positive effects to grow dramatically down the line as physicians, allied health care professionals, surgeons, and other hospital staff begin to take part.
Austria: The intensive care unit (ICU) wards in Vienna General Hospital produce upward of 35,000 pieces of raw data every day, all of it potentially key in catching hospital-acquired infections early, such as a rising count in inflammatory proteins or a reddening around a wound site. To harness the enormity of these numbers and make them a little more useful, the hospital has recently installed a smart surveillance system call Monitoring of Nosocomial Infections (MONI). MONI is an algorithm-based software developed by researchers at the Medical University of Vienna and the nearby clinical support company Medexter Healthcare. It’s designed to comb automatically through the available ICU information, run it against infection surveillance criteria definitions, and kick out alerts and reports when it detects early warning signs. An initial study published in 2012 pitted the system against manual ward surveillance in two ICU wards in the hospital. Manual surveillance missed 18 infection episodes and reported five false positives; assessing the same patients, the MONI software missed only four episodes, generated one false positive, and required 85% less time to do the job than the human. The MONI crew is now working on building interest and rolling the system out to other hospital systems in Austria and beyond.
“The computer is never tired,” says Klaus-Peter Adlassnig, a medical informatician at the Medical University of Vienna and the Medexter Healthcare chief executive officer. Granted, surveillance is only one small part of a hospital’s task, he says, but there are no limits to it. “It can take thousands of data [points]. You could establish a center and get data from the whole of Austria, the whole of Germany, and the technology would provide.”
Shannon Fischer is a freelance science writer living in Boston, Massachusetts.
[/accordion]
Design Considerations for the Intelligent Hospital
The design of an intelligent hospital must take into account several key considerations. It must balance the tradeoff between the complex technologies added to the environment with the enhancement of patient care and business benefit. The design needs to provide a high degree of automation, enabling validation checks and balances and alerts, independent of user compliance, and interaction with these systems. Supply management applications, such as those within the OR, validate the supply accuracy and establish methodologies to manage critical supplies, provide regulatory compliance, and optimize supplies throughout the hospital.
It is well documented that all RF systems have the potential to induce and are susceptible to electromagnetic interference (EMI). This can interfere with communications and the RFID tag reading process. Sometimes faulty equipment, such as an improperly working overhead light, can emit RF signals that interfere with the signal acquisition and impact the process. Of greater concern is that the RFID system itself may introduce EMI to other devices and systems, both hardwired and networked. Recent research has confirmed the potential of interference. This requires institutions to provide due diligence to test and evaluate this potential in their specific environments to ensure patient safety.
In conclusion, today’s health care environment increasingly relies on managing patients within the home. This will require hospitals to also develop provisions for monitoring and communicating with patients regardless of location. Telemedicine technologies create the opportunity for physiological parameters, medication compliance, and mobility to be dynamically reviewed. Consequently, the design of an intelligent medical home has started to reestablish centralized monitoring capabilities within the hospital, enabling clinical staff to dynamically follow up, interact, and assess patient progress, allowing for early warning of potentially undesirable or dangerous patient trends. Together, these systems work to bring health care into the 21st century, while at the same time improving the overall care of patients.



