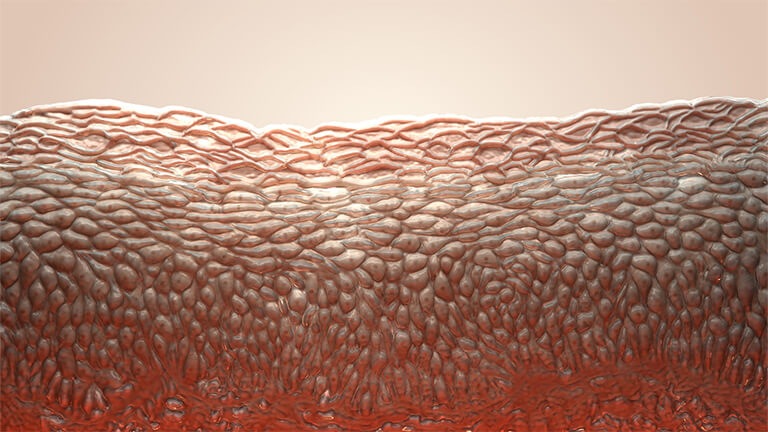
Human skin acts as a barrier between the body and the outside environment, preventing disease-causing organisms and foreign substances from getting into our body. The skin also serves as an ecosystem for billions of microorganisms, collectively called the skin microbiome. Some of these microorganisms are merely bystanders, while others work together with the skin to fight invaders or promote immunity. While knowledge of the skin microbiome lags behind that of the gut microbiome, there is growing evidence that microbial imbalances on the skin are associated with skin disorders and chronic wounds.
What’s living on our skin?
Heidi Kong is a dermatologist and head of the Cutaneous Microbiome and Inflammation Section at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (Figure 1). She was part of a team that conducted a metagenomic survey of 20 skin sites from healthy volunteers [1]. “The study showed that the skin microbiome tends to be very site-specific,” says Kong. “I cannot compare a swab from my forehead to a swab from your arm. They aren’t equivalent because the skin type is different.”
Kong and colleagues found that human skin is made up of many different habitats and microbial communities. There are three main types of skin microenvironments: sebaceous (or oily, like the face), moist (like armpits and belly buttons), and dry (like arms). Skin sites across the body vary in skin thickness and the density of hair follicles and glands. The researchers write that moist versus dry skin areas “are likely as ecologically dissimilar as rain forests are to deserts” [1].

Figure 1. Heidi Kong is a dermatologist and head of the Cutaneous Microbiome and Inflammation Section at the National Institute of Arthritis and Musculoskeletal and Skin Diseases. [Photo courtesy of Rhoda Baer (www.rhodabaerphotography.com/faces-of-science).]

Figure 2. Kong and colleague combine a traditional laboratory cultivation approach with metagenomic sequencing to create a collection of reference genomes for the human skin microbiome. [Photo courtesy of Rhoda Baer (www.rhodabaerphotography.com/faces-of-science).]
Beneficial bacteria
“The microbes on our skin have co-evolved with our body to help protect it and maintain health,” says Richard Gallo, a distinguished professor and the founding chairman of the Department of Dermatology at the University of California, San Diego, CA, USA (Figure 3). “One general theme is that they help to protect against pathogens and limit inflammation.”

Figure 3. Richard Gallo, distinguished professor and the founding chairman of the Department of Dermatology at the University of California, San Diego, CA, USA. (Photo courtesy of UCSD.)
Gallo and his team have found that two commensal species of Staphylococcus bacteria, S. epidermidis and S. hominis, secrete natural antibiotic molecules. These antibiotic molecules can disrupt the cell membranes of other bacteria, like the disease-causing S. aureus that frequently colonizes the skin of individuals with atopic dermatitis (also called eczema). The researchers also showed that bacterial strains producing these antibiotics were depleted in individuals with atopic dermatitis and the topical application of the strains could decrease S. aureus colonization [3].
Microbiologist Lindsay Kalan, of the University of Wisconsin, Madison, also studies the molecules that bacteria on our skin are producing and how they might be potentially harnessed as novel antimicrobials (Figure 4). She says that a healthy skin microbiome helps prevent pathogens from invading and colonizing the skin. “We think that is occurring by our commensal bacteria simply filling that niche and using up nutrients, but also by directly producing bioactive metabolites that could have antimicrobial properties, as well as other metabolites that participate in host-microbiome crosstalk,” says Kalan.
Indeed, several research groups have demonstrated that skin microbes play important roles in educating and regulating our innate immune response. Gallo’s team, for instance, showed that S. epidermidis produces a molecule that prevents inflammatory cytokine release from skin cells. Through this mechanism, the bacteria can help promote wound healing and reduce inflammation [4]. In another recent study, Gallo and colleagues found that S. epidermidis may also assist in protecting against skin cancer [5]. They discovered that certain strains of the microbe produce a molecule that can inhibit melanoma and other cancer cells in mice, while sparing healthy cells. It seems that about 20% of people carry this cancer-protective strain of S. epidermidis.

Figure 4. Microbiologist Lindsay Kalan, University of Wisconsin, Madison, studies the molecules that bacteria on our skin are producing and how they might be potentially harnessed as novel antimicrobials. (Photo courtesy of L. Kalan.)
Microbial dysbiosis and disease
While a properly functioning microbiome supports the immune system, destabilization of its equilibrium may contribute to several skin disorders, including acne and atopic dermatitis. This phenomenon, known as dysbiosis, alters the proportions of organisms in the skin microbiome and can be caused by internal and external stressors [6].
Acne, for example, is a common skin condition that occurs when lipids and dead skin cells clog hair follicles. It is associated with a skin microbiome unbalanced with lipophilic commensal bacteria like Cutibacterium acnes. Almost all adults are colonized with C. acnes but only a minority have acne, highlighting the important interactions between genetics, immune or barrier defects, the microbiome, and the environment [7].
Atopic dermatitis is also thought to have a bacterial component. Disease flare-ups are associated with increases in S. aureus and decreases in overall skin microbe diversity [8]. However, it is still unclear if these changes are a consequence of the disease or whether S. aureus contributes to disease initiation. “If you have more eczema-prone skin, is it more attractive for certain bacteria to attach and proliferate or are these bacteria exacerbating the skin disease?” says Kong. “If the bacteria are playing a role in exacerbating skin disease, then in addition to treating the inflammation, it might be important to also control the proliferation of this bacteria. But the jury is still out on that.”
As a dermatologist, Kong works with different patient populations, including those with primary immunodeficiencies. Part of her research involves investigating differences in atopic dermatitis in otherwise healthy people and patients with primary immunodeficiencies. Kong and her colleagues have found that immunodeficient patients tend to have more permissive skin; that is, they harbor more diverse microbe communities, including species not normally found on healthy adults [9]. In another study, the team demonstrated that patients with a particular primary immunodeficiency called DOCK8-deficiency have many more viruses in their skin microbiome than healthy individuals, whose microbiomes are primarily bacterial [10].
In addition to common skin diseases, skin microbes have also been shown to impact the healing of chronic wounds, such as those prevalent in the elderly and diabetic patients. In a longitudinal survey of microorganisms associated with diabetic foot ulcers, Kalan and her colleagues investigated how these microbial populations changed over time as treatments were applied [11].
“We found that stable bacterial communities were associated with poorer outcomes, while more dynamic change in the community suggested the wound was on a better trajectory and would heal faster,” she says. “I think this likely reflects that, as the wound is healing, the microenvironment is changing so we see a subsequent change in the microbial community.”
Factors impacting the skin microbiome
Microbial communities on the skin are influenced a great deal by the skin microenvironment but other intrinsic factors also come into play. Aging is associated with many changes in skin structure and topography, such as spot and wrinkle formation and modified sebaceous gland activity, which impact the ecological conditions at different skin sites [12]. Physiological differences between male and female skin environments have also been described, influenced by factors including hormone production, perspiration rate, and skin surface pH. And ethnicity seems to also play a secondary, but not insignificant, role in shaping the skin microbiome, partly through differences in lifestyle [13].
Since the skin surface is in direct contact with the external environment, extrinsic factors also impact the skin microbiome. A major contributor to variations in skin microbial communities between people is whether they live in rural or urban environments. Studies show that the diversity of the microbial community on skin decreases and its composition changes with increasing urbanization [13]. The impact of living environment on skin microbiota appears especially important in young children (1–4 years of age), compared to babies and older children. Such microbial differences may be due to different exposures to microorganisms associated with soil, water, and animals (both livestock and pets) [14]. Further research is needed to determine how the microbial ecology of the skin becomes established and stabilizes during the first years of life and how variations in early exposures may influence immune development and disease risk.
Exposure to antibiotic medication also appears to have repercussions for the skin microbiome. In one study, mice who were orally administered the antibiotic vancomycin had decreased bacterial density and altered bacterial composition in skin wounds, possibly contributing to delayed wound healing [15]. More recently, Kong and colleagues administered four different antibiotic regimens to healthy volunteers and sampled their skin microbiomes before, during, and up to one year after antibiotic use [16].
“With two of the antibiotic regimens, the healthy volunteers had Staphylococci bacteria on their skin that developed resistance to those antibiotics within a matter of days,” says Kong. “This antibiotic resistance persisted even after they stopped taking the antibiotic, through the length of the year-long study. Just one course of antibiotics triggered resistance which didn’t go away.”
During the COVID-19 pandemic, people were asked to wash and sanitize their hands more frequently; could this alter the skin microbiome? This is the subject of ongoing research but it seems that washing with soap or using alcohol-based sanitizers is effective at removing disease-causing microbes from the hands while having limited impact on skin microbiome diversity. However, too frequent disinfection may disrupt the microbiome by damaging the skin surface [13].
When it comes to cosmetics and other products applied to the skin, Kalan says it is unlikely that they affect one’s skin microbiome very much. “I often get asked if showering or using skin products on a daily basis impacts your microbiome and, so far, the evidence suggests that actually the skin microbiome is quite stable over time,” she says.
Targeting and treating the skin microbiome
Although there is still much to learn about the skin microbiome’s role in health and disease, there are already efforts underway to alter it by eliminating disease-causing species, transplanting beneficial species, or engineering microbes to reduce harm or increase benefits.
“Knowledge is progressing quickly,” says Gallo, whose team is involved in clinical trials designed to replace bacteria missing from patients with atopic dermatitis. They have developed a cream that contains strains of Staphylococcus found on human skin that inhibit S. aureus (the strain associated with flares of atopic dermatitis) by producing an antimicrobial compound [17].
Gallo says that “multiple phase 1 clinical trials have been very promising,” demonstrating the cream’s safety and efficacy in reducing S. aureus in individuals with atopic dermatitis. The latest results show that applying the cream twice a day for a week reduces S. aureus numbers by more than 99% and decreases symptom severity by 20%–30%. MatriSys Bioscience, a company cofounded by Gallo, is working to bring the cream to market in the next two to three years [8]
With the exception of a few cases, like S. aureus in atopic dermatitis, scientists still lack a detailed understanding of what differentiates healthy and diseased skin microbial communities. More research is needed before treatments targeting the skin microbiome come to drugstores and pharmacies. Kong says that current products that say they work to balance the skin microbiome are premature.
“What is a healthy skin microbiome?” she asks. “We have shown that in healthy individuals, there is a large range for what’s normal. When it comes to the skin microbiome, I think it is easier to identify what is aberrant, rather than what is normal.”
The skin is the human body’s largest organ and the first barrier between the body and the outside world. Our skin is home to numerous diverse microorganisms. While some of these microorganisms can promote immunity or fight invaders, other, disease-causing microbes sometimes invade the skin surface, causing damage, disease, and slow healing. Researchers are beginning to reveal the complexity of the microbial communities living on our bodies and establish the basis for new microbiome-targeting treatments to maintain healthy skin.
References
- E. A. Grice et al., “Topographical and temporal diversity of the human skin microbiome,” Science, vol. 324, no. 5931, pp. 1190–1192, May 2009, doi: 10.1126/science.1171700.
- S. S. Kashaf et al., “Integrating cultivation and metagenomics for a multi-kingdom view of skin microbiome diversity and functions,” Nature Microbiol., vol. 7, no. 1, pp. 169–179, Jan. 2022, doi: 10.1038/s41564-021-01011-w.
- T. Nakatsuji et al., “Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis,” Sci. Transl. Med., vol. 9, no. 378, Feb. 2017, Art. no. eaah4680, doi: 10.1126/scitranslmed.aah4680.
- Y. Lai et al., “Commensal bacteria regulate toll-like receptor 3-dependent inflammation after skin injury,” Nature Med., vol. 15, no. 12, pp. 1377–1382,
Dec. 2009, doi: 10.1038/nm.2062. - T. Nakatsuji et al., “A commensal strain of Staphylococcus epidermidis protects against skin neoplasia,” Sci. Adv., vol. 4, no. 2, Feb. 2018, Art. no. eaao4502, doi: 10.1126/sciadv.aao4502.
- V. Moskovicz, A. Gross, and B. Mizrahi, “Extrinsic factors shaping the skin microbiome,” Microorganisms, vol. 8, no. 7, p. 1023, Jul. 2020, doi: 10.3390/microorganisms8071023.
- A. L. Byrd, Y. Belkaid, and J. A. Segre, “The human skin microbiome,” Nature Rev. Microbiol.,
vol. 16, no. 3, pp. 143–155, Mar. 2018,
doi: 10.1038/nrmicro.2017.157. - E. Sohn, “Skin microbiota’s community effort,” Nature, vol. 563, no. 7732, pp. S91–S93, Nov. 2018,
doi: 10.1038/d41586-018-07432-8. - J. Oh et al., “The altered landscape of the human skin microbiome in patients with primary immunodeficiencies,” Genome Res., vol. 23, no. 12, pp. 2103–2114, Dec. 2013, doi: 10.1101/gr.159467.113.
- [10] O. Tirosh et al., “Expanded skin virome in DOCK8-deficient patients,” Nature Med., vol. 24, no. 12,
pp. 1815–1821, Dec. 2018, doi: 10.1038/s41591-018-0211-7. - M. Loesche et al., “Temporal stability in chronic wound microbiota is associated with poor healing,” J. Investigative Dermatol., vol. 137, no. 1, pp. 237–244, Jan. 2017, doi: 10.1016/j.jid.2016.08.009.
- M. Boxberger et al., “Challenges in exploring and manipulating the human skin microbiome,” Microbiome, vol. 9, no. 1, p. 125, Dec. 2021, doi: 10.1186/s40168-021-01062-5.
- K. Skowron et al., “Human skin microbiome: Impact of intrinsic and extrinsic factors on skin microbiota,” Microorganisms, vol. 9, no. 3, p. 543, Mar. 2021, doi: 10.3390/microorganisms9030543.
- C. Callewaert, K. R. Helffer, and P. Lebaron, “Skin microbiome and its interplay with the environment,” Amer. J. Clin. Dermatol., vol. 21, no. S1, pp. 4–11, Sep. 2020, doi: 10.1007/s40257-020-00551-x.
- M. Zhang et al., “Oral antibiotic treatment induces skin microbiota dysbiosis and influences wound healing,” Microbial Ecol., vol. 69, no. 2, pp. 415–421, Feb. 2015, doi: 10.1007/s00248-014-0504-4.
- J.-H. Jo et al., “Alterations of human skin microbiome and expansion of antimicrobial resistance after systemic antibiotics,” Sci. Transl. Med., vol. 13, no. 625, Dec. 2021, Art. no. eabd8077, doi: 10.1126/scitranslmed.abd8077.
- T. Nakatsuji et al., “Development of a human skin commensal microbe for bacteriotherapy of atopic dermatitis and use in a phase 1 randomized clinical trial,” Nature Med., vol. 27, no. 4, pp. 700–709, Apr. 2021, doi: 10.1038/s41591-021-01256-2.