Could biotechnology stop aging? The answer may be yes, no, or something in between, depending on who is being asked and what it means to “stop” aging. For those at one end of the spectrum— life extension seekers (including some deep-pocketed Silicon Valley investors)—the answer is “yes.” They believe biotechnology will lengthen human life spans to range anywhere from 1,000 years to forever. But for most, the answer is more nuanced and involves a dream of extended healthspan, rather than immortality. They imagine a future in which people over the age of 65 years are healthy, active, independent, and not burdened by disease, and that this is the norm rather than the exception. “Healthspanners” believe that one day, science will delay the onset of aging-related conditions and, as a side-effect, modestly extend life. Aging as we know it—and dread it—could become ancient history.
Age as a number one risk factor
Asking what the future holds for aging is neither idle nor esoteric. The “Silver Tsunami” is unfurling, increasing the urgency to address aging’s economic and social costs—whether by treating its conditions or slowing its advance. In the United States alone, about 10,000 people turn 65 every day. Eighty-five percent of people over the age of 65 years have at least one chronic disease associated with aging— cancer, arthritis, dementia, diabetes, and heart disease [1]. Age-related diseases tend to cluster, so developing one soon leads to another. As such, the majority of the over-65 population will develop two or more debilitating ailments as they age. It’s like a game of whack-a-mole, says Dr. Laura Carstensen in The Healthspan Imperative film—you might knock out one disease, but another often appears in short order. This clustering suggests that fundamental processes linked to the passage of time predispose people to these conditions.
A new approach to gerontology, “geroscience,” aims to address this clustering by researching how the aging process affects the disease process. If we don’t go after the root causes of aging, geroscience asserts, we are merely exchanging one disease for another. Dr. James Kirkland, who directs the Robert and Arlene Kogod Center on Aging at the Mayo Clinic, is blunt about the outlook for an aged patient: “If you cured any one age-related disease—for example, atherosclerosis, which causes heart attacks or strokes—you’re basically choosing to die of another one a few weeks or months later, such as Alzheimer’s or some cancer.” It would be great to find a cure for cancer, geroscientists agree, but what if you could suppress a whole suite of diseases at once, including cancer? The payoff in terms of increased life expectancy and quality for the general population would be multiplied.
Geroscientists believe their research will lead to compressed morbidity in old age, that is, a shortened period of decline before death. Extended healthspan is already experienced by a select group of people: centenarians. Many are active, mentally sharp, and enjoying life right to the end, with sometimes just a few weeks or days of dying. Dr. Laura Niedernhofer, director of the Institute on the Biology of Aging and Metabolism, University of Minnesota, is adamant about the goal of extending healthspan, more so than life span. Designing interventions that extend how long people live without guaranteeing they’re going to be healthy during that period of lengthened life is “the worst thing you could possibly do,” she says.
Although aging is a universal experience, researchers still don’t fully agree on how to categorize it. Although some talk about “curing” aging, that language is rejected by many since aging is a risk factor for many diseases, not a disease per se. Some define aging as a set of processes; others say it’s no process, but instead just widespread decay— increasing atrophy in everything (see “Breaking Down Aging” below).
[accordion title=”Breaking Down Aging”]
Dr. James Kirkland of the Mayo Clinic categorizes aging into four fundamental processes: chronic sterile inflammation, macromolecular and organelle dysfunction, stem- and progenitor-cell dysfunction, and cellular senescence. These four processes interact, Kirkland explains, and targeting any one of them (with a drug, for example), to speed it up or slow it down, tends to affect the others. Typically, these processes are upstream of the genesis of major chronic diseases such as diabetes, Alzheimer’s disease, most cancers, lung disease, liver disease, osteoarthritis, and osteoporosis. There’s also mounting evidence, Kirkland adds, that the four processes contribute to conditions of the geriatric syndromes, “things like frailty, age-related muscle impairment (sarcopenia), urinary incontinence, [and] mild cognitive impairment.” Lastly, they factor into a loss of resilience in older people—their decreased ability to withstand and rebound from events, such as the flu, surgery, fractures, or anesthesia.
[/accordion]
Despite the varying language, there’s a consensus that lifestyle modifications (e.g., quitting smoking), caloric restriction, and exercise can slow or mitigate certain aging processes. What’s new over the past 10 years is the discovery of drugs that target these fundamental aging processes and reduce a person’s risk of developing chronic disease. These drugs have the potential to extend human healthspan.
Targeting aging via senescence
Creaky joints, aches and pains, foggy brain—it’s the baggage of being old, but what is actually going on inside? These symptoms are caused by inflammation, Niedernhofer explains. There’s no infection present, she says, but the body feels like it has one because of senescence, a normally occurring program involving irreversible cell cycle arrest—which also happens to be a hallmark of aging.
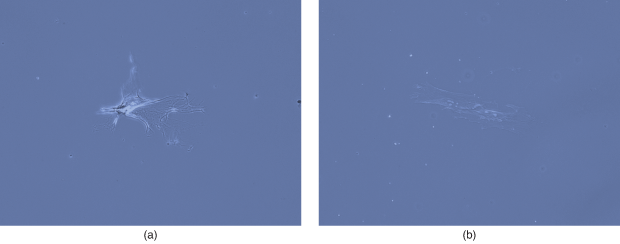
Cells that have undergone stress and can’t repair their DNA damage, for example, might either commit suicide (apoptosis) or enter senescence, which stops them from replicating so that they don’t create a mutated daughter cell. It’s a tumor suppressant mechanism that’s highly effective in young bodies, but which falters in older organisms. Senescent cells build up over time and the immune system becomes less efficient at clearing them [Figure 1(a) and (b)]. Meanwhile, they continue to secrete proinflammatory factors such as cytokines and chemokines—all intended, it’s believed, to flag the immune system for removal, but which, when not cleared, trigger damaging and painful inflammation. As one biotech company quips, senescent cells are like zombies—“they should be dead but they survive and cause havoc” [2].
Senescence has received attention from all corners: industry, research universities, and life extension movements; and research in this area is representative of the challenges and promise surrounding other elements of aging. Senescence has spawned a spectrum of theories from the speculative to the proven, prompted substantial investments from the private sector, and produced eye-widening discoveries in animal models. Each new finding fuels the recurring question of whether what is true for mice might also be true for humans.
It’s also at the top of investments by industry and academic institutions. In 2018, Unity Biotechnology amassed US$300 million in funding, with backing from tech moguls Jeff Bezos and Peter Thiel. The company is developing medicines to eliminate senescent cells in a bid to treat diseases that come with advanced age like inflammatory joint disease, atherosclerosis, pulmonary fibrosis, and chronic kidney disease. This business model for drug development— of targeting aging (via senescence in this case) while also linking outcomes to a specific disease(s)—is a bid to make a profit in the nearer term while pursuing aging research that will potentially be lucrative in the longer term.
Unity Biotechnology may be the exception more than the rule when it comes to securing outsized investments. In other cases, funding for senescence research is complicated by the traditional, and still dominant, paradigm of “one drug, one target, one disease.” Senolytics, drugs that target senescent cells for elimination, don’t fit this paradigm as they are often used in combination. They’re intended to go after networks rather than a single target, and to do this in parallel rather than in series. Working across different conditions, they have the potential to delay, prevent, or alleviate age-related diseases as a group. “It’s much more like developing an antibiotic than it is a drug that acts on a receptor in a normal cell,” offers Kirkland, suggesting that an old concept for a new class of drugs may help with understanding how antiaging drugs like senolytics work—a mindset shift the pharmaceutical industry has not yet made.
Senescence at the cellular level
Meanwhile, studies involving senescence in animal models are offering compelling evidence that it’s linked to age-related diseases, everything from Alzheimer’s to idiopathic pulmonary fibrosis to osteoporosis. “We found that transplanting even very small numbers of senescent cells is sufficient to cause age-related diseases,” says Kirkland of some of his laboratory’s recent work [3]. For example, if you inject 200,000 senescent cells, which is a tiny number, around the knee joint of mice, you will cause osteoarthritis in that knee joint, but not the opposite one.”
Senescence can spread from cell to cell and these “zombie” cells can kill cells around them while they remain resistant to dying. The effect, as it plays out in laboratory mice, can be dramatic. When Kirkland transplants small numbers of senescent cells into the abdomen of young mice, the mice “become frail,” he says. “They look old. They have trouble walking. … They have trouble hanging from wires. … They have trouble with treadmill endurance. They develop age-related diseases earlier as a group. They die early.” One of the more staggering findings Kirkland shares is how few senescent cells are required to have a negative effect. “If you transplant these cells such that in a mouse, a young mouse, only one in 10,000 cells in that mouse is a transplanted senescent cell, that’s enough to drive early death and early onset of age-related diseases,” he says.
Kirkland has developed senolytics based on the hypothesis that some anticancer drugs might also be able to clear senescent cells. These drugs work, not by damaging the cells, but by “transiently disabling the pathways that defend these cells against committing suicide,” Kirkland explains. Kirkland calls this a “hit-and-run” approach because the senolytics selectively eliminate a new crop of senescent cells while not interfering with the machinery that allows a cell to become senescent. Protecting senescence in certain contexts is important because it is beneficial during embryogenesis, early childhood development, and wound healing.
Mice that have had senescent cells removed appear rejuvenated and show signs of improved physical ability (Figure 2). In other words, removing senescent cells doesn’t just stop the advance of aging; it seems to reverse it.

In her lab at the University of Minnesota, Dr. Laura Niedernhofer has used aged animals/tissues to test specifically whether, when an organism already shows signs of aging, senolytics still work. “The answer was a resounding ‘yes,’” Niedernhofer reports. In one study, her laboratory treated aging mice with the senolytic fisetin, resulting in the restoration of tissue homeostasis and improved health of the liver and kidney. Age-related symptoms were reduced and life span was extended [4]. Fisetin also worked in human explants (biopsies taken during surgery of human tissue). In another study, the aged mice who received the senolytics to clear senescent cells showed signs of reversed physical dysfunction: They had greater endurance, strength, and speed [3]. The two studies, taken together, says Niedernhofer, “hold the greatest promise to date that this might be translatable from model systems or mice and into people.” Niedernhofer adds that the other potential benefit to these particular drugs is that they might have fewer side effects because they wouldn’t have to be taken daily. “You could [treat patients] periodically … say, every 2 months, and that would clear senescent cells. It takes about 60 days for you to accumulate more [senescent cells]. That would be a lot safer than giving a drug every day.”
But creating clinical trials to test agingrelated breakthroughs is, Niedernhofer points out, “a mind-bending” exercise that poses a host of design challenges: “Are you going to measure life span of people? When are you going to start giving the drug? Are you trying to prevent something, reverse something?” These questions and others are integral to answering whether or not biotechnology will ultimately transform in aging.
The first clinical trial to target aging
Several years ago, he and other geroscientists came up with the idea for the first clinical trial to determine if a drug can delay the multimorbidities of aging. Barzilai, director of the Institute for Aging Research, Albert Einstein College of Medicine, designed the study, Targeting Aging with Metformin (TAME), to serve as a template for future trials of aging-related treatments. Metformin is approved by the U.S. Food and Drug Administration (FDA) to help maintain balanced blood sugar levels in the body and is used to treat Type 2 diabetes, heart disorders, and polycystic ovary syndrome. Over time, it’s been seen that patients on metformin also experience delays in developing other age-related conditions and outlive nondiabetics.
Metformin isn’t the only FDA-approved drug for a specific condition that has the potential to also delay aging and extend life span, but in contrast to metformin, which is used by a large group of people, some other drugs are approved for the treatment of rare conditions. Growth hormone inhibitor is a medication prescribed to patients with acromegaly, a condition in which people have a pituitary adenoma that secretes growth hormone and which can be fatal if left untreated. Molecular biologist John Kopchick, who discovered the protein that inhibits growth hormone action, genetically engineered mice without the growth hormone receptor gene. These mice, in addition to being dwarf and fat, “were very resistant to the development of cancer and diabetes … and they were living extremely long.” One of Kopchick’s “mini” mice lived to age 5, double the average mouse life span. Since then, humans with a similar mutation in the growth hormone receptor have also shown traits of dwarfism and do not develop cancer. But even if the growth hormone inhibitor drug were FDA-approved for anything other than acromegaly, it’s expensive and must be injected daily, so it’s not currently feasible for use by a wider population.
For the more “mainstream” drugs such as metformin and rapamycin that treat one condition, but also seem to lengthen human healthspan, there are hurdles in moving these drugs through the necessary clinical trials for FDA-approved use for aging. Barzilai is planning to launch TAME this year, although the effort still has not raised the needed funding. “It’s an excruciatingly long process,” Barzilai says. The difficulty in advancing these clinical trials relates to the mindset shift referred to earlier. Funding institutions and private investors have yet to fully embrace geroscientists’ conviction that aging as a risk factor can be targeted in the same way that, for example, high cholesterol in heart disease can be targeted, even if the potential targets and outcomes would be multiplied.
Some wonder why a substance that is already FDA-approved can’t be rolled out at scale to stave off one or more other chronic diseases. Any researcher will tell you the risk is too great. “We have to go fast,” agrees James Kirkland, “but we can’t cut corners. We do not want people selfmedicating. We don’t want them going out and buying some of these supplements from health food stores and consuming massive amounts because it could be very dangerous.”
Despite the “cautious” pace at which the large-scale TAME has moved forward, promising (if preliminary) findings are coming in from smaller-scale trials. In early 2019, Kirkland’s team reported results from a first-in-human clinical trial of senolytics for treating idiopathic pulmonary fibrosis, an ultimately fatal lung disease associated with cell senescence [5]. “Five days after completing a course of 9 doses of senolytic drugs over a 3-week period,” Kirkland writes, “the 14 patients had significant improvements in walking distance, walking speed, ability to get into and out of a chair, and a short battery of physical function tests.” This small pilot study would need to be extended in time and numbers of participants (and have a placebo control group), but Kirkland says this type of study reaffirms “that interventions targeting aging processes may one day be used to treat formerly untreatable diseases and to extend healthspan.”
For researchers leading the way in aging research, the “big-picture” excitement at the prospect of treating previously incurable diseases is palpable. “The progress in one decade is extraordinary,” says Niedernhofer, “—from defining aging processes that are druggable, to identifying drugs, to creating a road map with the FDA (for clinical trials).” If the field and its potential impact were visualized, it might look like that famous surrealist painting, The Persistence of Memory, in which pocket watches melt off a tree branch and down the side of hard surfaces. Should biotechnology effectively disrupt human aging as we know it, it would be time and its effects that slowly melt away as the body ticks on, solid and steady.
References
- National Institute on Aging, “Supporting older patients with chronic conditions,” May 2017. [Online].
- Life Biosciences. Accessed: Mar. 4, 2019. [Online].
- M. Xu et al., “Senolytics improve physical function and increase lifespan in old age,” Nature Med., vol. 24, no. 8, pp. 1246–1256, 2018. [Online].
- M. J. Yousefzadeh et al., “Fisetin is a senotherapeutic that extends health and lifespan,” EBioMedicine, vol. 36, pp. 18–38, Oct. 2018. [Online].
- J. N. Justice, “Senolytics in idiopathic pulmonary fibrosis: Results from a first-in-human, open-label, pilot study,” EBioMedicine, 2018. [Online].



